Saphenion®: Covid-19 and varicose – a common cause of deep vein thrombosis and embolism
Saphenion®: Covid-19 and varicose: The risk factors for superficial venous thrombosis (OVT) are close to those for venous thromboembolism (VTE). The risk of these superficial skin vein thromboses is, however, a lot higher if varicose veins are already present (defective venous valves with the subsequent standing blood column and pathological reflux into the lower leg veins!)
This reflux increases the pressure in the deep veins to over 100 mmHg – and therefore there is already a high risk of thrombosis. Now a virus is added, which accumulates and multiplies in all inner walls of the vessel. This also applies to the vascular wall of varicose veins!
As can already be read everywhere, COVID-19 creates an inflammation of the vascular wall of the deep leg veins – this in itself has a thrombogenic effect.
However, the question must then be asked whether the varicose vein does not first become inflamed and the superficial thrombosis, which therefore develops very quickly, migrates into the deep veins of the leg that the virus has already inflamed. This then leads to the often fatal pulmonary embolism, most recently in Covid-19.
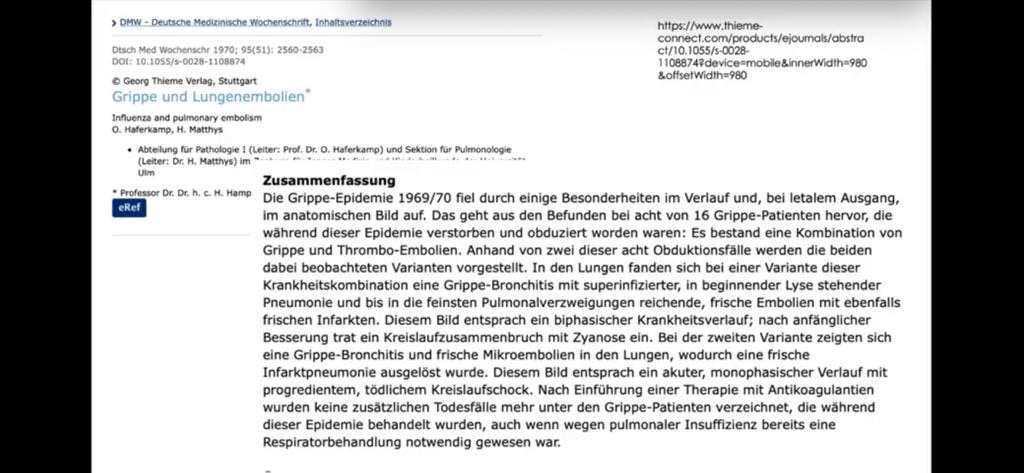
However, this pathological process was already discussed 50 years ago and can be found in our literature research for many older scientific articles.
Saphenion®: Covid-19 and varicose: common cause of deep vein thrombosis and embolism in Covid-19
Varicose veins are the main cause of OVT in the lower extremities, but underlying diseases that already exist (e.g. autoimmune diseases, infections, malignancy, or thrombophilia) must also be looked for in superficial vein thrombosis. A simultaneous deep vein thrombosis after skin vein thrombosis of varicose veins occurs in 15% of those affected. The severe complication of pulmonary embolism is seen in around 5% of those affected. However, these numbers do not yet take into account the pathological influence of various viruses (like Covid-19)!
Many viral infections (influenza, HIV, varicella, Covid-19) are associated with coagulation disorders. All aspects of the coagulation cascade, hemostasis, coagulation, and thrombosis resolution can be affected. As a result, thrombosis and bleeding can occur in all vascular regions. The examination of coagulation disorders as a result of various viral infections was not carried out consistently. Common paths have therefore not been fully clarified. For many severe viral infections, there is no treatment other than supportive measures. We have already proposed some options.
Saphenion®: Covid-19 and varicose – recommendation from a vascular surgical point of view
It is very important to us – as vascular surgeons – to point out that COVID-19 is not the first virus with these significant thromboembolic – sometimes fatal – side effects. There are other risk factors! And in any case, this includes the varicose veins, which are generally not considered so much from a disease perspective. From the point of view of the viral complication, these represent an easy point of attack and cause very rapid thrombosis and embolism.
As a result, there is an urgent recommendation to our patients not only to address this problem in times of viral pandemics. Function and cosmetics are important factors, complications due to varicose veins cannot be planned or predicted! This creates the recommendation for specialist diagnostics and necessary therapy with the various therapeutic methods recommended today.
Saphenion®: Covid-19 and varicose – a current patient history
In the middle of May 2023, a 61-year-old female patient with pronounced varicose veins presented in our practice. In the medical history, pneumonia due to pulmonary embolism in a coronavirus infection was found.
In the patient discussion, our patient reported several pre-operations on the varicose veins left. 6 and 7 years ago and in the recent past of superficial venous thrombosis in the area of recurrent varicose veins on the left leg. She then also had to be treated with deep vein thrombosis. Pneumonia appeared about 14 days after the deep vein thrombosis, the pulmonary embolism was initially not noticed by her. When admitted to a hospital in Berlin, the coronavirus infection was found.
The infection has now healed, and the deep veins have been recanalized – we have recommended to our patient that the skin vein system be restored using VenaSeal® vein glue and micro foam therapy.
Greetings to our Saphenion® – Senior Consultant, PD Dr. med. W.Lahl – Many Thanks for his suggestions and for sending older literature.

Photos: Saphenion®, Utzius
Links / References:
Khan R, Yasmeen A, Pandey AK, Al Saffar K, Narayanan SR. Cerebral Venous Thrombosis and Acute Pulmonary Embolism following Varicella Infection. Eur J Case Rep Intern Med. 2019;6(10):001171. Published 2019 Sep 20. doi:10.12890/2019_001171
Ramacciotti E, Agati LB, Aguiar VCR, et al. Zika and Chikungunya Virus and Risk for Venous Thromboembolism. Clin Appl Thromb Hemost. 2019;25:1076029618821184. doi:10.1177/1076029618821184
Oliveira GN, Basso S, Sevivas T, Neves N. Varicella complicated by cellulitis and deep vein thrombosis. BMJ Case Rep. 2017;2017:bcr2017221499. Published 2017 Sep 7. doi:10.1136/bcr-2017-221499
https://www.aerzteblatt.de/nachrichten/112427/Raetselhafte-Blutgerinnsel-bei-COVID-19-Patienten
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30937-5/fulltext
https://pubmed.ncbi.nlm.nih.gov/32339221/?from_term=Covid-19+and+thrombosis&from_pos=1
https://pubmed.ncbi.nlm.nih.gov/32311448/?from_term=Covid-19+and+thrombosis&from_pos=5
Hepatitis C Virus Infection and Risk of Venous Thromboembolism: A Systematic Review and Meta-Analysis –Karn Wijarnpreecha 1, Charat Thongprayoon 1, Panadeekarn Panjawatanan 2, Patompong Ungprasert 3Affiliations expand
PMID: 28611268; DOI: 10.5604/01.3001.0010.0279
De Novo Portal Vein Thrombosis in Virus-Related Cirrhosis: Predictive Factors and Long-Term Outcomes; Hitoshi Maruyama 1, Hidehiro Okugawa, Masanori Takahashi, Osamu YokosukaAffiliations expand
PMID: 23381015; DOI: 10.1038/ajg.2012.452
Review: Viral Infections and Mechanisms of Thrombosis and Bleeding; M Goeijenbier 1, M van Wissen, C van de Weg, E Jong, V E A Gerdes, J C M Meijers, D P M Brandjes, E C M van GorpAffiliations expand
PMID: 22930518; PMCID: PMC7166625; DOI: 10.1002/jmv.23354
https://pubmed.ncbi.nlm.nih.gov/22437808/?from_term=virus+and+thrombosis&from_page=2&from_pos=6
https://pubmed.ncbi.nlm.nih.gov/30477976/?from_term=virus+and+thrombosis&from_page=2&from_pos=7
https://pubmed.ncbi.nlm.nih.gov/24961747/?from_term=virus+and+thrombosis&from_page=4&from_pos=7
Karathanos C, Spanos K, Saleptsis V, Tsezou A, Kyriakou D, Giannoukas AD. Recurrence of superficial vein thrombosis in patients with varicose veins. Phlebology. 2016;31(7):489‐495. doi:10.1177/0268355515596475
Filis K, Kavantzas N, Dalainas I, et al. Evaluation of apoptosis in varicose vein disease complicated by superficial vein thrombosis. Vasa. 2014;43(4):252‐259. doi:10.1024/0301-1526/a000360
Nicolaides A, Hull RD, Fareed J, et al. Superficial vein thrombosis [published correction appears in Clin Appl Thromb Hemost. 2013 Jun;19(3):344] [published correction appears in Clin Appl Thromb Hemost. 2013 Jun;19(3):344-9]. Clin Appl Thromb Hemost. 2013;19(2):208‐213. doi:10.1177/1076029612474840s
Jerkic Z, Karic A, Karic A. Clinically silent deep vein thrombosis in patients with superficial thrombophlebitis and varicose veins at legs. Med Arh. 2009;63(5):284‐287.
Warot M, Synowiec T, Wencel-Warot A, et al. Can deep vein thrombosis be predicted after varicose vein operation in women in rural areas?. Ann Agric Environ Med. 2014;21(3):601‐605. doi:10.5604/12321966.1120610
van Rij AM, Chai J, Hill GB, Christie RA. Incidence of deep vein thrombosis after varicose vein surgery. Br J Surg. 2004;91(12):1582‐1585. doi:10.1002/bjs.4701
Decousus H, Epinat M, Guillot K, Quenet S, Boissier C, Tardy B. Superficial vein thrombosis: risk factors, diagnosis, and treatment. Curr Opin Pulm Med. 2003;9(5):393‐397. doi:10.1097/00063198-200309000-00009Bedienfeld umschalten: Yoast SEO
